File this one under “never knew this group existed but what a cool idea”: The Consumer Technology Association Foundation, a public foundation with the mission to link seniors and people with disabilities with technologies to enhance their lives. Yep, they exist and they published a report that found, among other things, that “meeting the needs of a growing aging population will require new technologies, partnerships, ideas, and business models.”
Ok, so that’s not much of a revelation to those of us entrenched in this field. But read on, it gets better.
The report, titled “Outthink Aging,” also examines how technology will empower seniors to live longer, healthier, and more independent lives by preventing fraud and abuse, providing greater social connectivity, and improving access to vital information and services. Reaching all of these goals remains to be seen but they are worthy.
Among the more salient points made in the report is that technology is just part of the answer to addressing the complex challenges of an aging population. More innovation is needed in our field and technology is just one piece of this puzzle. Amen, and as the report aptly notes, “the aging population is not a user group.”
Human needs are complex and not easily met through technological fixes alone, it further states. The trick is to engage this cohort by “leveraging technical innovation and human empathy to enhance the human experience.”
I’m not sure what engaging “human empathy” looks like, but I understand where they are going, and I would add that the best way to create new innovations that meet the needs of an aging population is to develop the technology with elders and individuals with disabilities—not just for them.
In addition to some great ideas about innovation and technology, the report also notes that activities of daily living are “activities that happen on the surface of day-to-day life.” The groups offer a new list of “core desires of an aging population,” as follows:
- Health: Access to high-quality healthcare encouraging both physical and cognitive wellbeing.
- Connection: Capability to stay in touch with loved ones and maintain an active role in their communities.
- Security: Ability to live safely in one’s home and have protections against theft and financial fraud.
- Dignity and Independence: Respect and control over direction of their lives.
Also notable is the fact that the CTA Foundation collaborated with IBM to create the report. IBM seems pretty happy about it: “[It] is an excellent example of the new types of relationships that will be necessary to meet the needs of the growing aging population,” Dr. Ruoyi Zhou, director of IBM Accessibility Research, says in a statement. He’s right—new types of relationships will be a crucial factor in addressing the needs of elders in useful and innovative ways.
Stephen Ewell, executive director of the CTA Foundation, is also on board. In the same statement, he asserts that “new partnerships between industry, nonprofits, academia, government, and the general public will form to accomplish these goals.” He’s right, and I’m happy to see that more and more folks are getting it.
In addition to innovative ideas and collaborations, the two groups conducted an informal poll at last year’s Consumer Electronics Show (N = 300 to 400) to gauge attendees’ concerns about the challenges of aging:
- 47 percent of respondents worry most about losing their memory and suffering from dementia as they age.
- 38 percent believe smart homes and the Internet of Things will best help manage the aging process.
- 35 percent believe discussing assisted/long-term care is the most difficult conversation to have with their parents.
The report also cites other research from the foundation showing that the U.S. market for active aging technology now encompasses 85 million Americans, representing a $24.4 billion market opportunity in 2015 that is expected to grow to $42.7 billion by 2020 (more from AARP’s report on the longevity economy HERE).
In conclusion, I believe this report is a great resource if you’re interested in dipping your toe into the field of aging services or if you are already in it and need a refresher or energizer on innovation and resources.
If you want a focused approach, facilitated by experts in the senior living field and candid feedback, contact Quantum Age today.
 m particularly excited about one individual on the OPTIMIZE agenda, Jennie Bucove, founder and CEO of
m particularly excited about one individual on the OPTIMIZE agenda, Jennie Bucove, founder and CEO of  se and had lived in multiple long-term care centers. “He had been kicked out of every facility because of his disease, so Mike decided to create a community on his own,” Bucove explains.
se and had lived in multiple long-term care centers. “He had been kicked out of every facility because of his disease, so Mike decided to create a community on his own,” Bucove explains.
 assuredness is that this reason holds true for most of us. One of the many challenges we face in this era of health care is accomplishing this task while meeting the myriad requirements necessary to be paid for our services.
assuredness is that this reason holds true for most of us. One of the many challenges we face in this era of health care is accomplishing this task while meeting the myriad requirements necessary to be paid for our services.
 viders had an electronic health record (EHR) adoption blueprint that guides them through the process, step by step, to implementation? That’s exactly what LeadingAge’s Center for Aging Services Technology (CAST) has done.
viders had an electronic health record (EHR) adoption blueprint that guides them through the process, step by step, to implementation? That’s exactly what LeadingAge’s Center for Aging Services Technology (CAST) has done.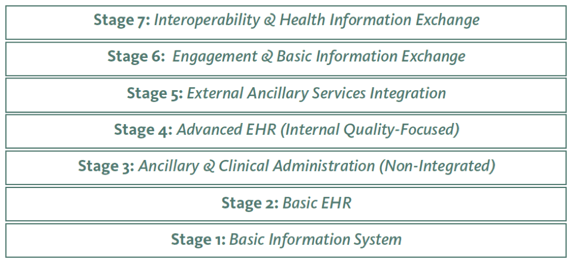 s new 7-Stage Adoption Model was tailored to help long-term care providers not only improve efficiency, but also quality of care for their residents.” He also said that he hopes the model will make it easier for more and more providers to integrate advanced EHR functionalities into their operations, and use them to continuously improve care quality.
s new 7-Stage Adoption Model was tailored to help long-term care providers not only improve efficiency, but also quality of care for their residents.” He also said that he hopes the model will make it easier for more and more providers to integrate advanced EHR functionalities into their operations, and use them to continuously improve care quality.