Bundled payments are here to stay—at least that’s the conclusion one may come to given some recent analyses of the topic. And if the powers that be at CMS read the latest Harvard Business Review, they would find some compelling arguments for making bundled payments a permanent fixture in the agency’s efforts to move Medicare into alternative payment models.
The article, “How to Pay for Health Care,” was particularly helpful in explaining why this model could be very successful in achieving the triple aim the agency aspires to. Authored by noted Harvard Professors Michael Porter and Robert Kaplan, the article offers some persuasive opinions about the potential that bundled payment models have in improving health care, reducing costs, and providing individualized care.
Within the context of long-term and post-acute care, there are two demonstrations under way that impact providers: the Comprehensive Care for Joint Replacement (CJR) model and the Bundled Payments for Care Improvement (BPCI) initiative.
In a bundled payment model providers are paid for the care of a patient’s entire care cycle—such as all services, procedures, tests, drugs, and devices used to treat a patient with a condition such as heart failure or a hip replacement, for example.
Bundled payments represent one component of CMS’ effort to boost value-based reimbursement, with capitation being the other. But Porter and Kaplan note that under capitation a provider must meet all the needs of a patient population with a fixed payment (per year, per covered life).
As the authors compare and contrast capitation and bundled payments, they are convinced that the solution to improving individualized health care and creating efficiencies will come with the latter. They liken bundled payments to a consumer’s experience purchasing products and services, where a single price is paid for a whole package that meets their needs—such as a car. With the purchase of a car, they argue, the consumer does not buy the motor from one supplier and the brakes from another—they buy a complete product from a single entity.
Bundled payments, they say, simply “draw on an approach long used in virtually every other industry.”
Among the arguments made against capitation is that it creates competition at the wrong level and on the wrong things, “rather than on what really matters to patients and to the healthcare system overall,” the authors state, noting that this is similar to how FFS models have traditionally worked. “Capitation rewards improvement at population level but not at individual level.” It is also not aligned with better or efficient care for each patient’s particular condition.
Another downside to capitation models: The risk factors are complex, which leads to an incentive for health systems to claim as many comorbidities as possible to bolster their revenue and profitability, they contend.
Porter and Kaplan conclude that capitation is wrong because it is a “top-down approach that achieves some cost savings by targeting low-hanging fruit such as readmission rates, expensive drugs, and better management of post-acute care.” The problem with this, they add, is that it doesn’t change how health care is delivered and neither does it hold providers accountable for efficiency and outcomes when it comes to patients and the treatment of their conditions. In short, it restricts patient choice and inhibits provider competition.
A recent analysis by consulting firm Avalere Health asserts that the increase in bundled payment models will impact LTPAC providers in several ways. Among them, will be fewer FFS patients, shorter lengths of stay, fewer readmissions, and a decreased use of costly settings
Avalere also has some predictions about bundled payments for the coming year and beyond: a reopening of the BPCI demonstration for new participants, a potential for new models, and an expansion of mandatory bundles like CJR.
Porter and Kaplan also state that bundled payments “will be the catalyst that finally motivates provider teams to work together to understand the actual costs of each step in the entire care process, learn how to do things better, and get care right the first time.”
These arguments could have a significant impact on healthcare delivery and LTPAC in particular. It’s worth the read.
 viders had an electronic health record (EHR) adoption blueprint that guides them through the process, step by step, to implementation? That’s exactly what LeadingAge’s Center for Aging Services Technology (CAST) has done.
viders had an electronic health record (EHR) adoption blueprint that guides them through the process, step by step, to implementation? That’s exactly what LeadingAge’s Center for Aging Services Technology (CAST) has done.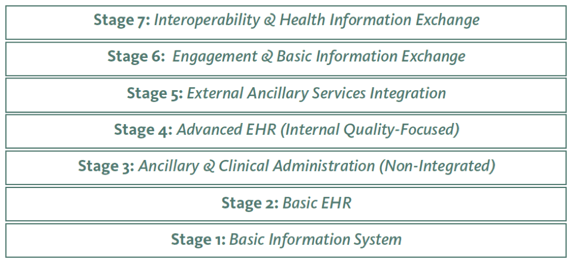 s new 7-Stage Adoption Model was tailored to help long-term care providers not only improve efficiency, but also quality of care for their residents.” He also said that he hopes the model will make it easier for more and more providers to integrate advanced EHR functionalities into their operations, and use them to continuously improve care quality.
s new 7-Stage Adoption Model was tailored to help long-term care providers not only improve efficiency, but also quality of care for their residents.” He also said that he hopes the model will make it easier for more and more providers to integrate advanced EHR functionalities into their operations, and use them to continuously improve care quality.